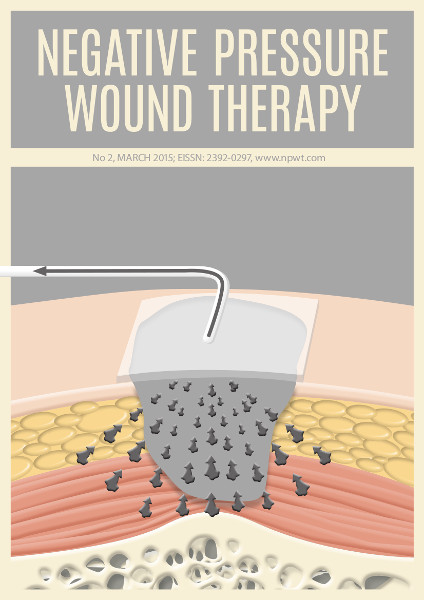
Modern alternative or first-line treatment: How to safely use Negative Pressure Wound Therapy in Diabetic Foot Syndrome?
Abstract
Clinical experience and basic science studies show that Negative Pressure Wound Therapy (NPWT) is a promising yet still under-used treatment method for patients with diabetic foot syndrome (DFS). Despite its advantages, it may carry the risk of serious side effects if the indications and contraindications are not strictly observed. The aim of this article is to discuss myths and facts about NPWT in conditions such as: inadequate blood supply, insufficient wound debridement, osteomyelitis or the necessity to monitor laboratory parameters during the therapy. We will try to define the optimal conditions for NPWT in order to obtain better results and eliminate the risk of side effects.
References
N. Singh, “Preventing foot ulcers in patients with diabetes,” JAMA,vol. 293, no. 2, p. 217 2005. http://dx.doi.org/10.1001/jama.293.2.217
R. Garg, K. Bajaj, S. Garg, P. Nain, and S. Uppal, “Role of negative pressure wound therapy in healing of diabetic foot ulcers,” Journal of Surgical Technique and Case Report, vol. 3, no. 1, p. 17 2011. http://dx.doi.org/10.4103/2006-8808.78466
P. Krasnodębski, A. Zoń, B. Mrozikiewicz-Rakowska, and W. Karnafel, “Ryzyko amputacji i umieralność osób z zaawansowanym zespołem stopy cukrzycowej – badanie obserwacyjne,” Medycyna Metaboliczna, vol. 17, no. 4, pp. 29–33 2013.
R. T. Greenlee, T. Murray, S. Bolden, and P. A. Wingo, “Cancer statistics, 2000,” CA: A Cancer Journal for Clinicians, vol. 50, no. 1, pp. 7–33 2000. http://dx.doi.org/10.3322/canjclin.50.1.7
S. Vig, C. Dowsett, L. Berg, C. Caravaggi, P. Rome, H. Birke-Sorensen, A. Bruhin, M. Chariker, M. Depoorter, R. Dunn, F. Duteille, F. Ferreira, J. F. Mart´ınez, G. Grudzien, D. Hudson, S. Ichioka, R. Ingemansson, S. Jeffery, E. Krug, C. Lee, M. Malmsjo, N. Runkel, R. Martin, and J. Smith, “Evidence-based recommendations for the use of negative pressure wound therapy in chronic wounds: Steps towards an international consensus,” Journal of Tissue Viability, vol. 20, pp. S1–S18 2011. http://dx.doi.org/10.1016/j.jtv.2011.07.002
S. O. Oyibo, E. B. Jude, I. Tarawneh, H. C. Nguyen, L. B. Harkless, and A. J. Boulton, “A comparison of two diabetic foot ulcer classification systems: The wagner and the university of texas wound classification systems,” Diabetes Care, vol. 24, no. 1, pp. 84–88 2001. http://dx.doi.org/10.2337/diacare.24.1.84
A. K. McNulty, M. Schmidt, T. Feeley, P. Villanueva, and K. Kieswetter, “Effects of negative pressure wound therapy on cellular energetics in fibroblasts grown in a provisional wound (fibrin) matrix,” Wound Repair and Regeneration, vol. 17, no. 2, pp. 192–199 2009. http://dx.doi.org/10.1111/j.1524-475X.2009.00460.x
C. Xia, A. Yu, B. Qi, M. Zhou, Z. Li, and W. Wang, “Analysis of blood flow and local expression of angiogenesis-associated growth factors in infected wounds treated with negative pressure wound therapy,” Molecular Medicine Reports 2014. http://dx.doi.org/10.3892/mmr.2014. 1997
M. S. Timmers, S. L. Cessie, P. Banwell, and G. N. Jukema, “The effects of varying degrees of pressure delivered by negative-pressure wound therapy on skin perfusion,” Annals of Plastic Surgery, vol. 55, no. 6, pp. 665–671 2005. http://dx.doi.org/10.1097/01.sap.0000187182.90907.3d
Y. Kasai, H. Nemoto, N. Kimura, Y. Ito, and N. Sumiya, “Application of low-pressure negative pressure wound therapy to ischaemic wounds,” Journal of Plastic, Reconstructive & Aesthetic Surgery, vol. 65, no. 3, pp. 395–398 2012. http://dx.doi.org/10.1016/j.bjps.2011.08.010
O. Borgquist, E. Anesater, E. Hedstr ¨ om, C. K. Lee, R. Ingemansson, and M. Malmsjo, “Measurements of wound edge microvascular blood flow during negative pressure wound therapy using thermodiffusion and transcutaneous and invasive laser doppler velocimetry,” Wound Repair Regen, vol. 19, no. 6, pp. 727–733 2011. http://dx.doi.org/10.1111/j1524-475X.2011.00741.x
O. Borgquist, R. Ingemansson, and M. Malmsjö, “The influence of low and high pressure levels during negative-pressure wound therapy on wound contraction and fluid evacuation,” Plastic and Reconstructive Surgery, vol. 127, no. 2, pp. 551–559 2011. http://dx.doi.org/10.1097/PRS.0b013e3181fed52a
M. L. Venturi, C. E. Attinger, A. N. Mesbahi, C. L. Hess, and K. S. Graw, “Mechanisms and clinical applications of the vacuum-assisted closure (VAC) device,” American Journal of Clinical Dermatology, vol. 6, no. 3, pp. 185–194 2005. http://dx.doi.org/10.2165/00128071-200506030-00005
C. E. Attinger, J. E. Janis, J. Steinberg, J. Schwartz, A. Al-Attar, and K. Couch, “Clinical approach to wounds: D??bridement and wound bed preparation including the use of dressings and wound-healing adjuvants,” Plastic and Reconstructive Surgery, vol. 117, no. SUPPLEMENT, pp. 72S–109S 2006. http://dx.doi.org/10.1097/01.prs.0000225470.42514.8f
G. S. Schultz, R. G. Sibbald, V. Falanga, E. A. Ayello, C. Dowsett, K. Harding, M. Romanelli, M. C. Stacey, L. Teot, and W. Vanscheidt, “Wound bed preparation: a systematic approach to wound management,” Wound Repair Regen, vol. 11, no. s1, pp. S1–S28 2003. http://dx.doi.org/10.1046/j.1524-475X.11.s2.1.x
B. S. Pukstad, L. Ryan, T. H. Flo, J. Stenvik, R. Moseley, K. Harding, D. W. Thomas, and T. Espevik, “Non-healing is associated with persistent stimulation of the innate immune response in chronic venous leg ulcers,” Journal of Dermatological Science, vol. 59, no. 2, pp. 115–122 2010. http://dx.doi.org/10.1016/j.jdermsci.2010.05.003
H. J. Wallace and M. C. Stacey, “Levels of tumor necrosis factor-α (TNF-α) and soluble TNF receptors in chronic venous leg ulcers – correlations to healing status,” J Investig Dermatol, vol. 110, no. 3, pp. 292–296 1998. http://dx.doi.org/10.1046/j.1523-1747.1998.00113.x
N. J. Trengove, H. Bielefeldt-Ohmann, and M. C. Stacey, “Mitogenic activity and cytokine levels in non-healing and healing chronic leg ulcers,” Wound Repair and Regeneration, vol. 8, no. 1, pp. 13–25 2000. http://dx.doi.org/10.1046/j.1524-475x.2000.00013.x
S. K. Beidler, C. D. Douillet, D. F. Berndt, B. A. Keagy, P. B. Rich, and W. A. Marston, “Multiplexed analysis of matrix metalloproteinases in leg ulcer tissue of patients with chronic venous insufficiency before and after compression therapy,” Wound Repair and Regeneration, vol. 16, no. 5, pp. 642–648 2008. http://dx.doi.org/10.1111/j.1524-475X.2008.00415.x
D. R. Yager, L.-Y. Zhang, H.-X. Liang, R. F. Diegelmann, and I. K. Cohen, “Wound fluids from human pressure ulcers contain elevated matrix metalloproteinase levels and activity compared to surgical wound fluids.” J Invest Dermatol, vol. 107, no. 5, pp. 743–748 1996. http://dx.doi.org/10.1111/1523-1747.ep12365637
R. Lobmann, A. Ambrosch, G. Schultz, K. Waldmann, S. Schiweck, and H. Lehnert, “Expression of matrix-metalloproteinases and their inhibitors in the wounds of diabetic and non-diabetic patients,”
Diabetologia, vol. 45, no. 7, pp. 1011–1016 2002. http://dx.doi.org/10.1007/s00125-002-0868-8
B. Mwaura, B. Mahendran, N. Hynes, D. Defreitas, G. Avalos, T. Adegbola, M. Adham, C. Connolly, and S. Sultan, “The impact of differential expression of extracellular matrix metalloproteinase inducer, matrix metalloproteinase-2, tissue inhibitor of matrix metalloproteinase- 2 and PDGF-AA on the chronicity of venous leg ulcers,” European Journal of Vascular and Endovascular Surgery, vol. 31, no. 3, pp. 306–310 2006. http://dx.doi.org/10.1016/j.ejvs.2005.08.007
S. McLennan, D. Min, and D. Yue, “Matrix metalloproteinases and their roles in poor wound healing in diabetes,” Wound Practice and Research, vol. 16, pp. 116–121 2008.
S. Mendez-Eastman, “Guidelines for using negative pressure wound therapy,” Advances in Skin & Wound Care, vol. 14, no. 6, pp. 314–323 2001. http://dx.doi.org/10.1097/00129334-200111000-00015
S. R. Young, S. Hampton, and R. Martin, “Non-invasive assessment of negative pressure wound therapy using high frequency diagnostic ultrasound: oedema reduction and new tissue accumulation,” International Wound Journal, vol. 10, no. 4, pp. 383–388 2012. http://dx.doi.org/10.1111/j.1742-481X.2012.00994.x
B. Bucalo, W. H. Eaglstein, and V. Falanga, “Inhibition of cell proliferation by chronic wound fluid,” Wound Repair Regen, vol. 1, no. 3, pp. 181–186 1993. http://dx.doi.org/10.1046/j.1524-475X.1993.10308.x
T. Phillips, H. al Amoudi, M. Leverkus, and H. Park, “Effect of chronic wound fluid on fibroblasts,” J Wound Care, vol. 7, p. 527–532 1998.
T. Weed, C. Ratliff, and D. B. Drake, “Quantifying bacterial bioburden during negative pressure wound therapy,” Annals of Plastic Surgery, vol. 52, no. 3, pp. 276–279 2004. http://dx.doi.org/10.1097/01.sap.0000111861.75927.4d
C. M. Moues, M. C. Vös, J. C. V. D. Bemd, T. Stijnen, and S. E. Hovius, “Bacterial load in relation to vacuum-assisted closure wound therapy: A prospective randomized trial,” Wound Repair and Regeneration, vol. 12, no. 1, pp. 11–17 2004. http://dx.doi.org/10.1111/j.1067-1927.2004.12105.x
M. Laato, J. Niinikoski, C. Lundberg, and B. Gerdin, “Inflammatory reaction and blood flow in experimental wounds inoculated with staphylococcus aureus,” European Surgical Research, vol. 20, no. 1,pp. 33–38 1988. http://dx.doi.org/10.1159/000128738
S. M. Levenson, “Wound healing accelerated by staphylococcus aureus,” Arch Surg, vol. 118, no. 3, p. 310 1983. http://dx.doi.org/10.1001/archsurg.1983.01390030042007
E. Yusuf, X. Jordan, M. Clauss, O. Borens, M. Mader, and A. Trampuz, “High bacterial load in negative pressure wound therapy (NPWT)foams used in the treatment of chronic wounds,” Wound Repair Regen,vol. 21, no. 5, pp. 677–681 2013. http://dx.doi.org/10.1111/wrr.12088
S. Jeffrey, “Advanced wound therapies in the management of severe military lower limb trauma: a new perspective,” Eplasty, vol. 9, p. e28 2009.
P. E. Campbell, G. S. Smith, and J. M. Smith, “Retrospective clinical evaluation of gauze-based negative pressure wound therapy,” International Wound Journal, vol. 5, no. 2, pp. 280–286 2008. http://dx.doi.org/10.1111/j.1742-481X.2008.00485.x
M. Kaufman and D. Pahl, “Vacuum-assisted closure therapy: wound care and nursing implications,” Dermatol Nurse, vol. 4, pp. 317–25 2003.
J. Bickels, Y. Kollender, J. C. Wittig, N. Cohen, I. Meller, and M. M. Malawer, “Vacuum-assisted wound closure after resection of musculoskeletal tumors,” Clinical Orthopaedics and Related Research, vol. 441, pp. 346–350 2005. http://dx.doi.org/10.1097/01.blo.0000180450.21350.3e
M. Shirakawa and R. R. Isseroff, “Topical negative pressure devices,” Arch Dermatol, vol. 141, no. 11 2005. http://dx.doi.org/10.1001/archderm.141.11.1449
P. Stanirowski and W. Sawicki, “Nowoczesne metody terapii trudnogojacych sie połozniczo- ginekologicznych ran pooperacyjnych- analiza ˙przydatnosci i skuteczności stosowania,” Postepy Nauk Medycznych, vol. 7, pp. 475–487 2013.
J. Apelqvist, K. Bakker, W. H. van Houtum, and N. C. Schaper, “Practical guidelines on the management and prevention of the diabetic foot,” Diabetes Metab. Res. Rev., vol. 24, no. S1, pp. S181–S187 2008. http://dx.doi.org/10.1002/dmrr.848
S. McCallon, C. Knight, J. Valiulus, M. Cunningham, J. McCulloch, and L. Farinas, “Vacuum-assisted closure versus saline-moistened gauze in the healing of postoperative diabetic foot wounds,” vol. 46, no. 8, pp. 28–32 2000.
“Consensus statement on negative pressure wound therapy (v.a.c. therapy) for themanagement of diabetic foot wounds,” Ostomy Wound Management, vol. Suppl, pp. 1–32 2006.
M. Yuan-Innes, C. Temple, and M. Lacey, “Vacuum-assisted wound closure: a new approach to spinal wounds with exposed hardware,” Spine (Phila Pa 1976), vol. 26, no. 3, pp. E3–E4 2001.
C. Moues, G.-J. van den Bemd, W. Meerding, and S. Hovius, “An economic evaluation of the use of TNP on full-thickness wounds,” J Wound Care, vol. 14, no. 5, pp. 224–227 2005. http://dx.doi.org/10.12968/jowc.2005.14.5.26776
B. E. Leininger, T. E. Rasmussen, D. L. Smith, D. H. Jenkins, and C. Coppola, “Experience with wound VAC and delayed primary closure of contaminated soft tissue injuries in iraq,” The Journal of Trauma: Injury, Infection, and Critical Care, vol. 61, no. 5, pp. 1207–1211 2006. http://dx.doi.org/10.1097/01.ta.0000241150.15342.da
D. G. Armstrong and L. A. Lavery, “Negative pressure wound therapy after partial diabetic foot amputation: a multicentre, randomized controlled trial,” The Lancet, vol. 366, no. 9498, pp. 1704–1710 2005. http://dx.doi.org/10.1016/S0140-6736(05)67695-7
T. Hurd, P. Chadwick, J. Cote, J. Cockwill, T. R. Mole, and J. M. Smith, “Impact of gauze-based NPWT on the patient and nursing experience in the treatment of challenging wounds,” International Wound Journal, vol. 7, no. 6, pp. 448–455 2010. http://dx.doi.org/10.1111/j.1742-481X.2010.00714.x
C. A. Park, A. J. Defranzo, M. W. Marks, and J. A. Molnar, “Outpatient reconstruction using integraTMand subatmospheric pressure,” Annals of Plastic Surgery, vol. 62, no. 2, pp. 164–169 2009. http://dx.doi.org/10.1097/SAP.0b013e31817d87cb
S. D. Ramsey, K. Newton, D. Blough, D. K. McCulloch, N. Sandhu, G. E. Reiber, and E. H. Wagner, “Incidence, outcomes, and cost of foot ulcers in patients with diabetes,” Diabetes Care, vol. 22, no. 3, pp. 382–387 1999. http://dx.doi.org/10.2337/diacare.22.3.382
J. Apelqvist, D. G. Armstrong, L. A. Lavery, and A. J. Boulton, “Resource utilization and economic costs of care based on a randomized trial of vacuum-assisted closure therapy in the treatment of diabetic foot wounds,” The American Journal of Surgery, vol. 195, no. 6, pp. 782–788 2008. http://dx.doi.org/10.1016/j.amjsurg.2007.06.023
[1] N. Singh, “Preventing foot ulcers in patients with diabetes,” JAMA,vol. 293, no. 2, p. 217 2005. http://dx.doi.org/10.1001/jama.293.2.217
Copyright (c) 2015 Beata Mrozikiewicz-Rakowska, Ewelina Bucior, Joanna Kania, Adrianna Nowak, Marek Chojnowski, Janusz Krzymień

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
- Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal.
- Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgement of its initial publication in this journal.
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See The Effect of Open Access).
We require authors to sign a Publication Agreement prior to publication of the manuscript in NPWTJ. The link to this form may be found below.
PUBLICATION AGREEMENT FORM